FHIR Profiling Guidelines
Inhoud
Introduction
FHIR requires profiling. To do profiling in a comparable way we need conventions. This page lays out these conventions.
The created profiles are generally based on the Health and Care Information models (HCIM) defined by the program ‘Registratie aan de bron’ (Data capture at the point of Care) for the Netherlands. In the Netherlands, these models are more commonly known by the name zorginformatiebouwstenen or ZIB's. In this text, we make use of the HCIM abbreviation. The section Associating functional definition to StructureDefinition provides more information regarding these information models.
Canonical URL
Any conformance resource needs a canonical URL. This preferably leads somewhere but does not have to be processable. Canonical URL's are about the identity of artifacts, not necessarily about retrieval location. URIs for the latter (for artifacts living in ART-DECOR) are described in ART-DECOR FHIR_URIs.
For Nictiz profiles we SHALL use the following structure:
- For profiles:
- that are HCIM related (this should be the majority of profiles):
http://[domain]/fhir/StructureDefinition/zib-[English HCIM name] - standard specific:
http://[domain]/fhir/StructureDefinition/[project]-[name]
- that are HCIM related (this should be the majority of profiles):
- For extensions:
- pertaining to 1 HCIM:
http://[domain]/fhir/StructureDefinition/zib-[English HCIM name]-[English HCIM concept name] - not pertaining to HCIMs, and standard specific:
http://[domain]/fhir/StructureDefinition/[project]-[name] - pertaining to multiple HCIMs, or not pertaining to HCIMs and generally applicable:
- if the use context is a single resource:
http://[domain]/fhir/StructureDefinition/[resource]-[purpose] - otherwise:
http://[domain]/fhir/StructureDefinition/[purpose]
- if the use context is a single resource:
- pertaining to 1 HCIM:
- For value sets related to HCIMs:
http://decor.nictiz.nl/fhir/ValueSet/[value set OID]--[effective date as yyyymmddhhmmss]
Where:
- [domain] is "nictiz.nl"
- [project] is preferably the same as its matching ART-DECOR project prefix
- [purpose] is generally a camelCased name starting with a lowercase letter
This convention aligns with international initiatives such as DAF and QiCore and has been confirmed/advised by Grahame Grieve.
Versioning intro
The HL7® FHIR® specification specifies a lot of things related to versions. This text aims to stay aligned with the latest insights. Readers should first get acquainted with the core FHIR specification before reading here: http://hl7.org/fhir/versions.html
Versions of the profiles
Versions of the profiles may occur for any of the following reasons:
- New releases of the underlying HCIMs are normally followed by an update to the representing profiles
- Identified issues in existing profiles may require an update
- HL7® FHIR® updates may lead to an update of the profiles. We do not automatically follow every FHIR version as it is released
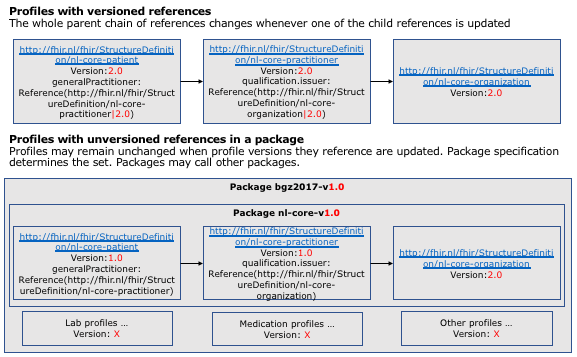
Version updates first and foremost affects the version element found in all conformance resources (profiles, value sets, extensions, search parameter, operation definition etc.). The update normally does not affect the canonical URI of the conformance resource. Conformance resources create a web of interrelated artifacts. Any resource that references another resource, e.g. Patient referencing Practitioner for the general practitioner, normally does so without a version indicator (uri|version). This means that any reference points dynamically to 'the latest version' of the artifact. If you were to build a consistent set of versions you would need to add the version to any reference in the set of conformance resources and update the full set after any updating any particular part.
Around the advent of FHIR R4, the follow up of STU3, there will be a new versioning layer that allows packaging of profiles into a consistent set without affecting the profiles itself. The packaging mechanism will be tested in May 2018, and should greatly simplify specification and implementation of versions.
Versions in instances
To understand how instances of resources are interpreted by a receiving server we should look at two things:
- The indicator for the profile that the sender added to the instance (if any). This indicator would be in the
Resource.meta.profileelement and may include a version, e.g.
<profile value="http://fhir.nl/fhir/StructureDefinition/nl-core-patient"/> - The profile (versions) that the server defaults to in the absence of a profile indicator in the instance
If the server does not support the profile (version) as indicated in the instance it may do any of the following things. See also the relevant section in the FHIR specification.
- Try to support the instance based on what it can support. This may lead to ignoring any element it doesn't know, except for modifierElements. If modifier elements are encountered, the instance should be rejected
- Reject the instance
Note: as specified in the core FHIR specification, the server SHALL use its CapabilityStatement to indicate its behavior around unsupported elements (ignore or reject)
Associating functional definition to StructureDefinition
Any StructureDefinition that profiles a Resource does so because there is some kind of logical definition dictating how. These functional definitions are known as Clinical Building Blocks, Health and Care Information Models or in Dutch Zorginformatiebouwstenen or zibs. Profiles SHALL have a traceable relationship with their functional counterpart(s).
The FHIR specification contains several solutions for this problem, ConceptMap (>=STU1), StructureMap (>=STU3), ElementDefinition.mapping. Neither of these solutions are mature and cover our use case.
- ConceptMap: works best for value sets and codes.
- StructureMap: overcomplicated and unclear how to apply and whether or not this has a future.
- ElementDefinition.mapping: is a free text mapping inside the profile. This means we cannot add mappings to profiles from third parties without updating their resource.
Current implementation
We use the mapping elements in profiles to map functional elements to resource elements. When slicing, the mapping is made on the content of the slice, not the slice itself (see also #Placing-Info).
Functional elements are referenced based on their mnemonic id in the HCIM, e.g. NL-CM:9.6.19936. The mapping shall resolve to the English page on zibs.nl:
<mapping>
<identity value="hcim-medicationagreement-v1.0-2017EN" />
<uri value="https://zibs.nl/wiki/MedicationAgreement-v1.0(2017EN)" />
<name value="HCIM MedicationAgreement-v1.0(2017EN)" />
</mapping>
....
<element id="MedicationRequest.extension:usageDuration">
<path value="MedicationRequest.extension" />
<mapping>
<identity value="hcim-medicationagreement-v1.0-2017EN" />
<map value="NL-CM:9.6.19936" />
</mapping>
</element>
Proposed way forward
- The functional definitions live in ART-DECOR and every concept in this functional definition has a versioned id.
- The technical FHIR profile elements we want to map to have an optional @id attribute, but according to Tracker#9843 it is a required item for profiles (StructureDefinition)
- In our own profiles we can make sure we populate this Element/@id and associate the functional concept on id / id basis. We found that DAF Profiles populate these ids as well.
- Example: <element id="Patient:DAF-Patient.extension:race">...</element>
- Example: <element id="2.16.840.1.113883.3.1937.99.62.3.2.3--20110128000000">
- In profiles we reference from third parties that do not have this Element/@id populated we need a less precise method. We will deal with that when we need to.
Practical guidelines
File names
- For profiles: <<the final part of the canonical URI>>.xml
- For valuesets: <<Valueset.name>>-<<Valueset.id>>.xml
Profile meta data
- URL: see above
- Resource ID: final part of the canonical URI
- Name: final part of the canonical URI (without hyphens, capitalized)
- Description:
- A(n) <<enter resource type>> resource as defined by the Dutch Health and Care Information models (Dutch: Zorginformatiebouwsteen or ZIB) <<Zorginformatiebouwsteen name>> <<version>> <<release>>
- Followed by the 'Concept' section from the HCIM
- Version: as applicable to the profile, not the HCIM it refers to
- Date: n/a
- Lifecycle status: as applicable (normally draft or active)
- Experimental: normally false or null
- Title: final part of the canonical URI (without hyphens, with 'zib' replaced by 'HCIM')
- Purpose:
- 'Purpose' section from HCIM
- If needed: a discussion of where this profile fits in the workflow and why this resource was chosen (separated using a header in Markdown)
- Copyright: CC0
- Publisher: Nictiz
- Contact information: n/a
- Use context: n/a
- Keywords: n/a
- Mappings: uri to the version of the HCIM specification (see #Associating_functional_definition_to_StructureDefinition)
<mapping>
<identity value="hcim-contactperson-v3.1-2017EN"/>
<uri value="https://zibs.nl/wiki/ContactPerson-v3.1(2017EN)"/>
<name value="HCIM ContactPerson-v3.1(2017EN)"/>
</mapping> - Identifiers: n/a
- Meta data: tbd
- Implicit rules (URI): n/a
- Language: n/a (most content is en-US from the core, some is nl-NL from the HCIMs)
- Kind: n/a (auto handled by Forge)
- Type: n/a (auto handled by Forge based on selection at creation time)
- Abstract: false
- Base definition: n/a (auto handled by Forge based on selection at creation time)
- FHIR version: n/a (auto handled by Forge based on selection at creation time) - initially 3.0.1 STU3
Mapping DefinitionCodes
Sometimes a FHIR element is equivalent to the HCIM concept (like a comment and a Resource.comment element), but if not, a code (usually SNOMED or LOINC) needs to be added to the FHIR profile to provide the proper definition. This is for example the case in Observation, where the root concept of the observation is unknown unless it is defined by the .code element, and where every .component needs to be defined by an individual .code element. Usually, the concepts for these elements are provided by the HCIMs (as DefinitionCode).
We map these DefinitionCodes from the HCIM onto the profile in an extendable way. If possible, we use a required slice for the DefinitionCode. In practice this will look like:
| FHIR path | Remark | Cardinality | |||
|---|---|---|---|---|---|
| .code | 1..1 | ||||
| .coding | sliced on value/code | 1..* | |||
| slice for concept | named after the concept name | 1..1 | |||
| .system | code system from HCIM as fixedValue | 1..1 | |||
| .code | code from HCIM as fixedValue | 1..1 | |||
| .display | display value defined in the code system as defaultValue | 0..1 | |||
Slicing definitions
Choosing the discriminator
Defining the discriminator should be based on the most specific slice definition as possible while keeping a close eye on performance cost. Use patterns instead of a combination of fixed values to keep the discriminator logic simple. For example when slicing the Coding/CodeableCocept datatype: use a pattern slice if the code and system of a slice are fixed. If the slices are discriminated by different CodeSystems then a discriminator based on a fixed system is preferred over a ValueSet binding. Use the latter if multiple CodeSystems can be used within a slice definition. Try to avoid the discriminator type 'profile' as this is a very costly operation for a validator.
Don't use nested slicing
In some cases, slicing in this way would mean to add slices within slices (e.a. Observation.component). This doesn't work too well in FHIR - for example, neither the Java nor the .Net validator can't handle this (at the moment) - so we don't use this mechanism. As an alternative, we can use a slicing discriminator based on pattern/code, and on each slice.code we can add a patternCodeableConcept with the required system and value. This has the same effect; at least that coding is required, but others may be added.
Binding HCIM defined ValueSets
- the ValueSet can be obtained in FHIR 3.0 format from ART-DECOR (see #File_names for file naming conventions)
- the reference URL can be obtained from the <<ValueSet.url>> element in this file
- we use binding strength "extensible".
- the <<binding.description>> value is set to <<ValueSet.name>>
Binding of HCIM BasicElements to profiles
The BasicElements were made explicit in HCIM Release 2017 and have been declared applicable to 2015 and 2016 in the zibs.nl wiki.
Initially, the profiles did not dedicate much attention to the BsasicElements as there was no clarity around how to interpret them. That clarity has since been added but there is still room for interpretation:
|
All HCIM's implicitly contain a number of basic elements. These are usually not included in the information models of the individual building blocks but are supposed to be present. These are concepts that are of a more technical nature, often have little or no clinical relevance, but are necessary for the sake of clarity and readability of the information. In those cases where these elements are of clinical significance, they will usually be explicit in the information models. An example of this is an AGB number as an identification number for a health professional. |
For some elements it's clear, e.g. the IdentificationNumber will always go to .identifier, and for other elements it is not, e.g. InformationSource. What would be the InformationSource for the resource Patient? When would a ContactPerson be a Subject in the current profiles, instance had of a Patient?)
The table outlines which mappings are clear and which are yet to be determined. As of the Spring release 2019 of MedMij, all BasicElement mappings have applied for as far as possible:
| BasicElement | Profiel element | Remark |
|---|---|---|
| NL-CM:0.0.1 HCIMRoot | - | not possible |
| NL-CM:0.0.6 IdentificationNumber | .identifier | Overlaps sometimes with existing mapping such as HealthProfessionalIdentificationNumber or PatientIdentificationNumber. Unclear what to do with sub parts of an HCIM such as LabroatoryTest and Specimen. Presumably best to map to Observation.identifier and Specimen.identifier |
| NL-CM:0.0.2 InformationSource | .asserter | Mapped only when clinically relevant, e.g. AllergyIntolerance.asserter, Condition.asserter. What HCIM is this really applicable to? |
| NL-CM:0.0.3 PatientAsInformationSource::Patient | Patient | |
| NL-CM:0.0.4 HealthProfessional | Practitioner | PractitionerRole | |
| NL-CM:0.0.5 RelatedPersonAsInformationSource::ContactPerson | RelatedPerson | |
| NL-CM:0.0.7 Author | .author | .performer | |
| NL-CM:0.0.8 PatientAsAuthor::Patient | Patient | |
| NL-CM:0.0.9 HealthProfessionalAsAuthor::HealthProfessional | Practitioner | PractitionerRole | |
| NL-CM:0.0.10 RelatedPersonAsAuthor::ContactPerson | RelatedPerson | |
| NL-CM:0.0.11 Subject | .subject | .patient | A RelatedPerson is never a Subject of care except possibly for a family anamnesis. Is it clinically relevant and/or reasonable to assume RelatedPerson as possible subject regardless? |
| NL-CM:0.0.12 Patient | Patient | |
| NL-CM:0.0.13 RelatedPersonAsSubject::ContactPerson | RelatedPerson | |
| NL-CM:0.0.14 DateTime | .effective | .onset | Is this clinically relevant time to be assumed only on clinical HCIMs? So not on e.g. Patient, Practitioner, Organization? |
Miscellaneous
- We only profile elements, cardinalities and bindings that require profiling. We leave other elements, cardinalities and bindings as-is (see #Open_vs._Closed_Modeling)
- For elements that map to Health and Care Information Models (HCIM):
- We copy the name from the HCIM element into the profile element.short (in elements that refer to other zibs, the name is built up like <<ElementName::ReferenceZibName>>, but we only use the part before the double colons)
- The HCIM concept description is placed in the profile element.definition
- The HCIM Dutch concept name is placed in the profile element.alias
- Note: as a rule of thumb, we place this info 'as close as possible' to the elements that actually represent the data. For example: when slicing, the texts are placed on the slice content, not the slice itself. Similarly, in concept containers like Observation.component, this info is placed on the .valueXXX elements. This is also true for the HCIM mappings.
- Implementation guidance, such as mapping clarification and usage, of HCIM concepts that are mapped to multiple elements is given on the root of the resource. The nl-core-address profile provides a good example.
- Slices get an UpperCamelCased name based on the HCIM element name.
- New elements defined through extensions get a lowerCamelCased name based on the HCIM element name.
- When adding invariants we use "hcim-[hcim-name]-[number]" as a key. Example: hcim-alert-1
- FHIR URI Strategy (draft document with potentially good info)
- For FHIR base resource elements with datatype code and binding required it may be that the HCIM has other/additional codes to specialize the FHIR codes. To conform to FHIR and the HCIM:
- We will document the mapping in a ConceptMap, which will be linked from the element .mapping comment.
- We will use the extension http://nictiz.nl/fhir/StructureDefinition/code-specification:
- The extension is of datatype CodeableConcept, which also supports text as a fallback. It is bound with strength "extensible" on the HCIM derived ValueSet in the profile where it is applied.
- The extension slice is named after the full English name of the code list according to the HCIM.
- Mapping from the HCIM concepts is applied to the .valueCodeableConcept.mapping in the extension (in addition to the .mapping in the FHIR element).
Open vs. Closed Modeling
| × | Open | Closed |
|---|---|---|
| Pros | - Forward compatibility
- Modelers don't have to think about what you shouldn't support, only what must be supported - Implementers can fit more data, even if it's not in specified explicitly bu the profile |
- Implementers, don't have to support all elements that maybe, someday could be used, according to the model
- Model becomes more specific - Model becomes smaller and more straightforward - More implementer feedback, about elements they want to support, but currently can't |
| Cons |
- Implementers, have to support all optional elements that maybe, someday could be used, according to the model - Model becomes more vague, - Model becomes larger and less straightforward about what should actually be supported, and what can optionally be supported - Less implementer feedback: elements they want to send can be easier 'hacked' in a not yet explicitly specified element. Model won't be improved. |
- More versions of models, after more elements have to be supported - No forward compatibility, only backwards - Implementers have to wait for a new version of the model, if they want to support elements, that are currently not in scope. |
We have chosen for "open" modeling for the HCIMs, since they are very general and not meant for one specific use case. Excluding unspecified elements here is not an option, since we expect derived profiles for more specific use cases that may need those elements.
Cardinality/conformance mapping table
Cardinality applies to the number of occurrences that an element MAY/SHOULD/SHALL have. Minimum cardinality is integer 0. Maximum cardinality is "n" or "*" (exact character depends on tooling). If the minimum cardinality is higher than 0, then an element has to be present.
Conformance applies to what a system MAY/SHOULD/SHALL support. When data for an element is missing, e.g. because it is not applicable, then the element may be absent, but when conformance MustSupport is active, then a conformant application SHALL support it. Contrary to V3, there is no concept of NullFlavor in FHIR, so whenever an element is 1..1 in FHIR, there is no escape through NullFlavor: a value SHALL be present.
Reference: ElementDefinition.mustSupport
This poses a need for a mapping table from cardinality/conformance in HCIMs versus that in profiles.
| Generic (HCIM) | FHIR | --- | Specific application | FHIR |
|---|---|---|---|---|
| 0..1 | 0..1 | 0..1 | 0..1 | |
| 0..1 C | 0..1 | 0..1 C | 0..1 | |
| 0..1 R | 0..1 | 0..1 R | 0..1 - consider mustSupport='true' | |
| 0..* | 0..* | 0..* | 0..* | |
| 0..* C | 0..* | 0..* C | 0..* | |
| 0..* R | 0..* | 0..* R | 0..* - consider mustSupport='true' | |
| 1..1 | 0..1 | 1..1 | 0..1 | |
| 1..1 C | 0..1 | 1..1 C | 0..1 | |
| 1..1 R | 0..1 | 1..1 R | 0..1 - consider mustSupport='true' | |
| 1..1 M | 1..1 | 1..1 M | 1..1 - consider mustSupport='true' | |
| 1..* | 0..* | 1..* | 0..* | |
| 1..* C | 0..* | 1..* C | 0..* | |
| 1..* R | 0..* | 1..* R | 0..* - consider mustSupport='true' | |
| 1..* M | 1..* | 1..* M | 1..* - consider mustSupport='true' |
mustSupport="true" has the consequence that any conformant instances based on this profile SHALL support this part of the profile in the way that is defined by the implementation guide that governs the profile. This is not possible to state for a generic profile that aims to support many more use cases/contexts than is possible to know from the perspective of the profile. If a specific context requires use of a certain part of the profile it MAY choose to specify a constraining profile on top of the generic profile to do just that.
Constraining references
HCIMs might have have connections to other HCIMs. Example: a MedicationAgreement might have a Prescriber relationship defined using a HealthProfessional which is mapped to a FHIR MedicationRequest.requester as Reference(Practitioner). The FHIR MedicationRequest however, defines more types: Reference(Practitioner | PractitionerRole | Organization | Patient | RelatedPerson | Device). The closed world model would mandate that the profile only marks Practitioner for use. The open world model would mandate that the profile describes that for a HealthProfessional you need the Practitioner without omitting the other choices.
For general purpose profiles, suitable for further constraining we use open world profiling meaning that we do not constrain the choices of references into just the types that the HCIM requires. We only constrain the generic resource reference to the generic profile(s) for that resource. For Practitioner this would be the nl-core-practitioner. If deemed relevant a second layer of derived profile(s) could be created to tailor the generic profile for a specific use case using closed world modeling.
Data type mapping table
DECOR defines a set of data types. In most cases, the mapping to FHIR is straightforward, though there are a number of cases which are not as clear-cut. When defining extensions, or specifying the datatype of an Observation or Questionnaire.item in FHIR, a mapping to the relevant FHIR datatype needs to be done. The table below shows a mapping for datatypes in HCIMs versus those in profiles.
| HCIM | ART-DECOR | FHIR | Remarks |
|---|---|---|---|
| INT | count | Count or integer | Count in FHIR is derived from Quantity, this is appropriate for observations, such a a count of red blood cells in a specimen. Count in FHIR is a Quantity with system="http://unitsofmeasure.org" and code="1" (for units). If this is not appropriate, use integer. |
| BL | boolean | boolean | |
| ED | blob | base64Binary | |
| CD | code | CodeableConcept or coding or code | In general, CodeableConcept will be the right choice. See Using Codes in Resources for details. |
| ANY | complex | BackboneElement | 'complex' is data which is not further defined in DECOR, and thus cannot be translated. |
| - | currency | Money | Does not have a HCIM counterpart currenty. Theoretically this could be MO |
| - | date | date | Does not have a HCIM counterpart currently. Closest counterpart could be TS |
| TS | datetime | dateTime | |
| - | decimal | decimal | Does not have a HCIM counterpart currently. Theoeratically this could be REAL |
| - | duration | Duration | Does not have a HCIM counterpart currently. Closest counterpart could be PQ |
| II | identifier | Identifier | |
| CO | ordinal | CodeableConcept or coding or code | See Using Codes in Resources for details. |
| ST | string | string | |
| - | ratio | Ratio | Does not have a HCIM counterpart currently. Closest counterpart could be RTO |
| - | text | string | Does not have a HCIM counterpart currently. |
| PQ | quantity | Quantity |
Translating DECOR to FHIR
Status: proposal
Quite often we will populate FHIR artifacts from DECOR artifacts. In such cases, FHIR identification must be derived from DECOR identification.
DECOR uses the attributes id and effectiveDate to identify concepts, datasets, transactions, valueSets and templates. The artifacts with the same id but different effectiveDates are subsequent versions of the same artifact (though artifacts can also get a new id for a new version, such as when a new dataset is derived from an older one).
In FHIR, every resource can have an id, which is the "logical id" of the resource. This id never changes once assigned, like DECOR id and effectiveDate. Resources usually have an URL too, which also identifies the resource, but should be resolvable. The URL can contain the id.
The following ART-DECOR artifacts map to FHIR artifacts:
| DECOR artifact | FHIR artifact | FHIR identifier system | Notes |
|---|---|---|---|
| concept | DataElement | http://art-decor.org/ns/oids/de | DataElement is a wrapper around a FHIR element (based on ElementDefinition). A FHIR element is not serializable independently, but is wrapped in a StructureDefinition or DataElement. |
| dataset transaction |
Logical Model | http://art-decor.org/ns/oids/sd | A Logical Model is a StructureDefinition without base resource. FHIR uses this to capture user requirements. |
| valueSet | ValueSet | http://art-decor.org/ns/oids/vs |
The following FHIR attributes are constructed in the following way, when generated from ART-DECOR. Non-digits are stripped from the timestamp in @effectiveDate because they violate the FHIR rules for id.
| FHIR artifact | derivation from DECOR |
|---|---|
| FHIR id | @id + '--' + @effectiveDate |
| FHIR identifier system | See above |
| FHIR identifier value | @id |
| FHIR version | @effectiveDate |
| FHIR status | See below |
Status is translated from DECOR to FHIR:
| DECOR status | FHIR status |
|---|---|
| new | draft |
| draft | draft |
| pending | draft |
| active | active |
| review | draft |
| cancelled | retired |
| rejected | retired |
| deprecated | retired |